Health
Immunocompromised people make up nearly half of COVID-19 breakthrough hospitalizations – an extra vaccine dose may help

The U.S. Food and Drug Administration and Centers for Disease Control and Prevention officially recommended on Aug. 12 and Aug. 13, 2021, respectively, that people who are moderately to severely immunocompromised receive a third dose of the COVID-19 vaccine.
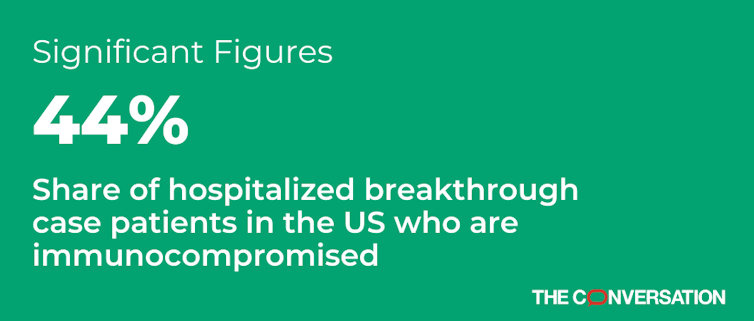
One reason for this recommendation is high hospitalization rates among immunocompromised people who are vaccinated. As of July 2021, nearly half of the vaccinated people hospitalized with breakthrough COVID-19 infections were immunocompromised – despite making up only 2.7% of the U.S. adult population. In comparison, the rate of breakthrough cases among vaccinated people who are not immunocompromised was less than 1%.
I am a physician scientist specializing in infections in immunocompromised patients. As someone who researches autoimmune disease and has worked on the COVID-19 vaccine trials, I agree that a third dose of COVID-19 vaccine can help protect those with weakened immune systems.
What does it mean to be immunocompromised?
People who are immunocompromised have weakened immune systems. This can result from certain diseases and their medical treatments, such as cancer, autoimmune diseases, untreated HIV, organ transplant medications and some forms of kidney disease. The common thread is that the body’s defenses against infection are impaired.
Two parts of the immune system seem to be particularly important in protecting people from getting sick with COVID-19: T cells and B cells. B cells make antibodies that can bind to and inactivate viruses. T cells kill off virus-infected cells, prevent infection from further spreading and organize the body’s overall defense response. Different types of immunocompromising conditions and treatments can either kill or decrease the effectiveness of these key immune cells.
That can result in a hampered response to vaccines. As a result, people who are immunocompromised often need to follow different vaccination guidelines from people who are not immunocompromised to best protect themselves from infection. After a bone marrow or solid organ transplant, for instance, patients are routinely revaccinated against such infections as hepatitis B.
COVID-19 is particularly dangerous for the immunocompromised
Early on in the pandemic, researchers learned that immunocompromised people infected with COVID-19 tend to have particularly severe and long-lasting infections. This leads to prolonged viral shedding, meaning that the period during which these infected people release the virus as they breathe, talk and eat is much longer. Thus, they have a higher chance of transmitting the virus to others.
Long infections with poor immune responses are also ideal environments for the virus to evolve and adapt in ways that allow it to better infect people.
While immunocompromised people were not included in the initial COVID-19 vaccine trials to avoid putting them at risk, subsequent studies revealed that the authorized two-dose mRNA vaccine regimens do not stimulate as strong a defense against COVID-19 for immunocompromised people. In particular, organ transplant recipients seem to develop fewer COVID-19 antibodies after vaccination. That’s not surprising, given that the medicines used in transplantation intentionally hamper antibody development to prevent the immune system from rejecting the donated organs. But since then, pilot trials in organ transplant recipients have shown that an additional dose of vaccine can help boost immune response.
The best protection for everyone against COVID-19 is to have as many people vaccinated as soon as possible. In the interim, a third vaccine dose can safely and effectively decrease the likelihood of severe COVID-19 in immunocompromised people. And consistently wearing masks, regardless of vaccination status and whether or not you’re immunocompromised, can also significantly reduce the spread of COVID-19.
[Get our best science, health and technology stories. Sign up for The Conversation’s science newsletter.]![]()
Jonathan Golob, Assistant Professor of Infectious Disease, University of Michigan
This article is republished from The Conversation under a Creative Commons license. Read the original article.





















