Health
Premature babies are prone to impaired brain development, but nutrients may reduce the risk

Extreme preterm birth is associated with impaired brain development: defective executive function, disruptive behaviours and psychiatric issues are more common among those born preterm than those born at term. This risk is greater at lower gestational ages.
The current global incidence of preterm birth is 11 per cent. With advancements in care before and after birth, an increasing number of extreme preterm (below 28 weeks of gestational age) babies survive. However, this increasing survival does not come with a reduction in the impaired brain development associated with premature birth.
As a neuroscience and nutritional biochemistry researcher, my focus is nutrition, neonatal brain development and associated brain disorders. Optimizing nutrition is a promising avenue: our research suggests that creatine, an energy-providing nutrient, may help mitigate the adverse brain development of these preterm babies.
Premature babies and nutrition
Premature infants often have immature digestive systems that aren’t ready to absorb adequate nutrients. As a result, they often depend on nutrients delivered intravenously, bypassing the digestive system. This method of feeding is called parenteral nutrition.
Creatine is a natural compound that is produced mainly in the kidneys and liver from three amino acids, the fundamental building blocks of proteins: arginine, glycine and methionine.
Healthy term babies receive nine per cent of their creatine requirements from their mother’s milk. These healthy babies produce the remaining requirement of creatine in their bodies.
Unlike human milk, newborn parenteral nutrition solutions do not routinely contain creatine, which leaves newborn premature babies dependent on their own production to meet their creatine requirement.
In healthy term babies, the majority of arginine, a building block of creatine, is produced in intestinal cells. However, feeding via the baby’s veins bypasses the intestine, so intravenous feeding interferes with normal arginine production. Because these premature babies cannot make enough arginine, they can’t make their required creatine.
Creatine and neurodevelopment
Creatine provides quick, short-term energy to skeletal muscles and heart. Muscle stores most of the body’s creatine (95 per cent), but the brain stores the second-highest amount. The brain is also the body’s second-highest energy user, after muscle.
The brain needs a continuous energy supply, and certain regions of our brains rely on creatine for energy. In the adult brain, interruption of this energy supply impairs brain function and leads to the progression of neurodegenerative diseases such as Parkinson’s, Alzheimer’s or Huntington’s diseases.
Creatine is also an important modulator of brain neuron systems, making it crucial for babies’ brain development. Babies born with inherited creatine deficiency disorders are not able to produce creatine. These babies experience frequent seizures, significant impairment in cognition, language development, upper or lower limb movements and behaviour problems. These outcomes clearly suggest the importance of creatine for normal brain function and development.
Supplementing creatine in parenteral nutrition solutions
Human studies provide limited information on the long-term metabolic consequences of the complete absence of creatine in parenteral nutrition solutions. An animal model such as piglets is ideal to study this situation. Our research showed neonatal piglets receiving parenteral nutrition intravenously for two weeks (which represents nine months for a human baby) did not sustain optimal creatine accumulation.
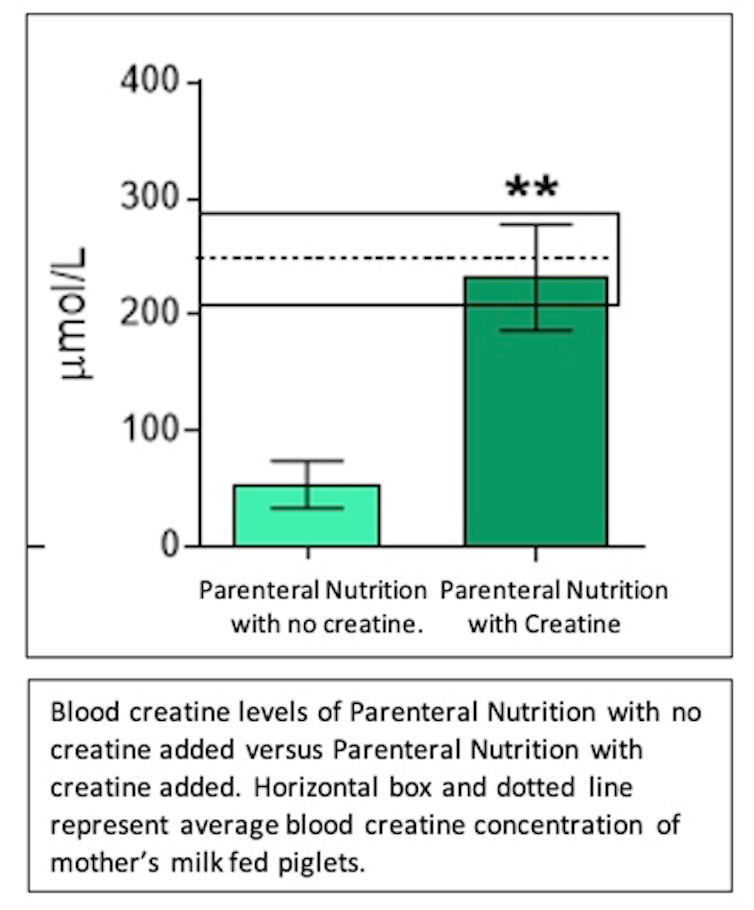
When creatine was added to the piglets’ parenteral feeding solution, piglets’ creatine accumulation improved.
To address the inadequate arginine production associated with complete intravenous feeding, some premature human infants are fed small amounts of parenteral nutrition solution into their stomachs via a tube. (This is a form of enteral nutrition — enteral means via the digestive tract and parenteral means outside the digestive tract — but similar feeding solutions are sometimes used for both ways of providing nutrition.) The remainder of the parenteral nutrition solution is delivered intravenously. However, because organ levels of creatine cannot be tested in human babies without damaging organs or risking health, human studies are of limited value in assessing this approach.
We fed the parenteral nutrition solution into the stomachs of our piglets. These neonatal piglets were not able to meet normal levels of creatine accretion without pre-made creatine in their parenteral nutrition solutions, even when the parenteral nutrition solution was delivered to their stomachs.
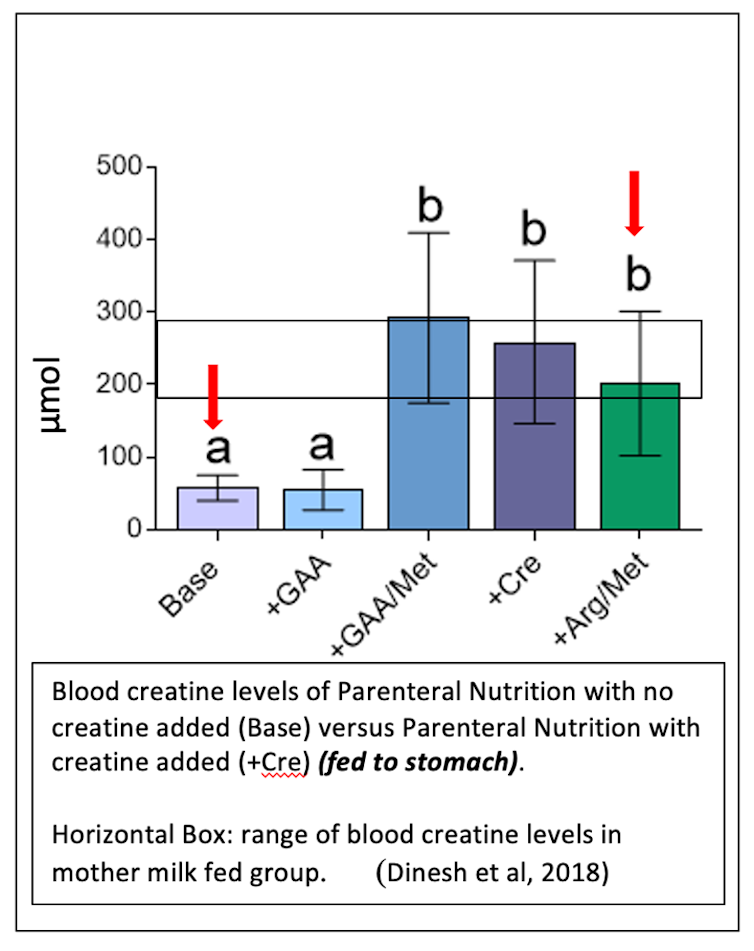
Piglets fed parenteral solution to their stomachs with no pre-made creatine had very low levels of creatine in their blood. However, piglets fed parenteral solution to their stomach with pre-made creatine or extra building blocks (arginine and methionine) improved their creatine levels. These levels were similar to the creatine levels of piglets fed mothers’ milk.
Our findings were supported by a recent review on human babies that concluded that hospital preterm babies need adjustments to nutritional components in order to achieve normal brain development.
Premature babies rely on parenteral and/or enteral nutrition support during their stay at hospital. However, creatine is not a routine component of these newborn parenteral/enteral nutrition solutions.
Supplementing these nutrition solutions with creatine to increase or regulate local energy stores and to regulate neuromodulation may help protect the developing brain. This approach represents a therapeutic tool for reducing the risks of developing abnormal neurological conditions in premature babies. Furthermore this approach may reduce the incidence of neurodegenerative diseases later in life of those born premature.![]()
Olupathage Chandani Dinesh, Postdoctoral Researcher (Department of Psychology) & Course Instructor (Department of Biochemistry), Memorial University of Newfoundland
This article is republished from The Conversation under a Creative Commons license. Read the original article.





















