Breaking
One dose, then surgery: A new way to test brain tumor drugs
Lori Simons took the bright orange pill at 3 a.m. Eight hours later, doctors sliced into her brain, looking for signs that the drug was working.
She is taking part in one of the most unusual cancer experiments in the nation.
With special permission from the Food and Drug Administration and multiple drug companies, an Arizona hospital is testing medicines very early in development and never tried on brain tumors before.
Within a day of getting a single dose of one of these drugs, patients have their tumors removed and checked to see if the medicine had any effect. If it did, they can stay on an experimental drug that otherwise would not be available to them. If it did not, they can try something else, months sooner than they normally would find out that a drug had failed to help.
“They don’t lose any time,” said Dr. Nader Sanai, the doctor leading the study at Phoenix’s Barrow Neurological Institute.
Time is everything for people with glioblastoma, the most common and deadly type of brain tumor, the kind that killed Massachusetts Sen. Edward M. Kennedy in 2009. Even when surgeons think they got it all, the cancer usually grows back and proves fatal. The few drugs to treat these tumors have little effect – median survival is about 14 months.
“We’ve had an endless string of failures” to find better ones, Sanai said.
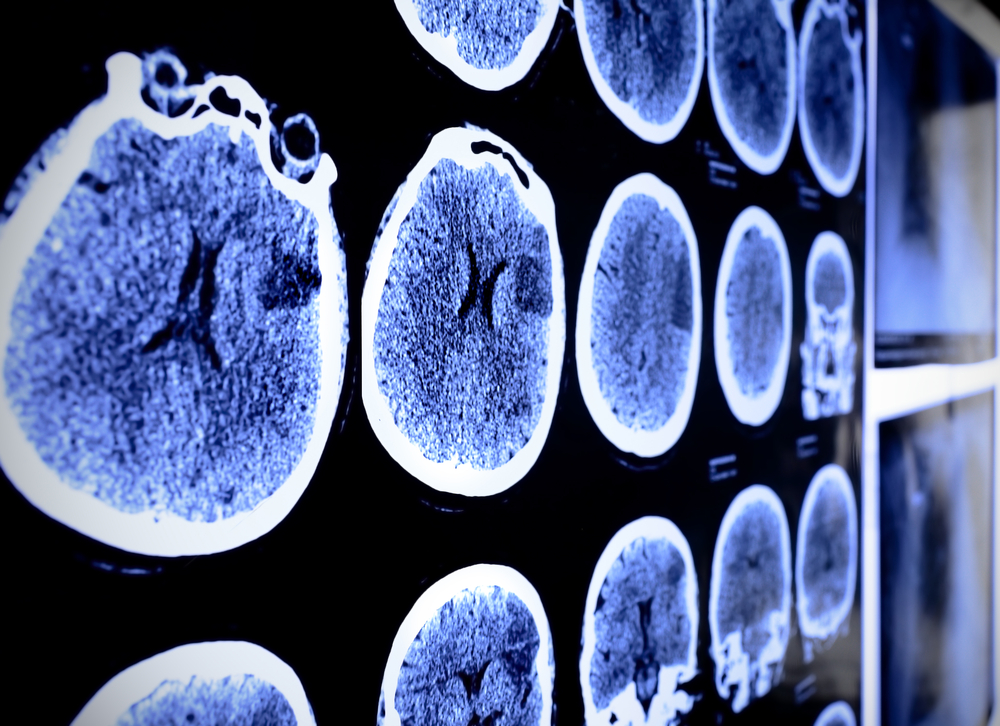
His study is for people whose cancer came back. Doctors use a stored sample from the original tumor to see if its growth is driven by any genes or pathways targeted by one of the experimental drugs in development. If so, they give that single dose of the new drug before surgery to remove the new tumor.
Then, the tumor tissue is examined under a microscope to see if the drug had its intended effect on the genes or pathways.
So far, the study has tested one drug from AstraZeneca PLC in four patients. Another drug, from Novartis, will be added soon.
“We’re trying to develop a portfolio of these” so there are many possible drugs available for new patients under a single “umbrella” study, Sanai said.
It is called a “phase zero” clinical trial because it comes before the usual three-phase experiments to determine a drug’s safety, ideal dose and effectiveness.
“We view this as a great thing, as something that will produce better drugs that have greater chance of working,” said Dr. Richard Pazdur, cancer drug chief at the FDA.
“Cost potentially will go down and certainly time will go down” for companies testing new drugs this way and patients seeking something that will help, he said.
Finding treatments for brain tumors is “a huge unmet medical need” that justifies trying a new approach, Pazdur said.
Dr. James Doroshow was involved in the only previous studies like this, done at the National Cancer Institute.
In the past, “if you had a new drug, you’d give it to a patient, you’d measure the blood levels, but very rarely would you have a way to know whether the presumed method of action was working in the patient,” he said.
The Arizona study gives a way to check that, because the tumor is removed right after the first dose is given. And if the drug does not work in any or few of the people who get it, the study could spare others a futile treatment, and limit the time and money a drug company invests.
“If you’re going to fail, you want to fail early and fail fast before you put thousands of patients into randomized trials,” Doroshow said.
The experimental drug did not appear to help Simons, a 55-year-old former pharmacist from Gold Canyon, an hour’s drive east of Phoenix. Doctors decided to try an older drug, Temodar, after her surgery in late October.
“The real interest in these kind of trials is not necessarily putting patients on these drugs but keeping them off drugs that aren’t going to work,” said Sanai, who treated Simons.
The patient said she had no regrets about participating.
“It’s a revolutionary trial. I think it will open up a pathway for many other drugs to be studied in this manner,” Simons said. “I go into this with no motive for me. It’s just for the future, people who have cancer like I do, and see what kind of treatments they can have.”