Science
Lungs have their own microbiome – and these microbes affect the success of bone marrow transplants in kids
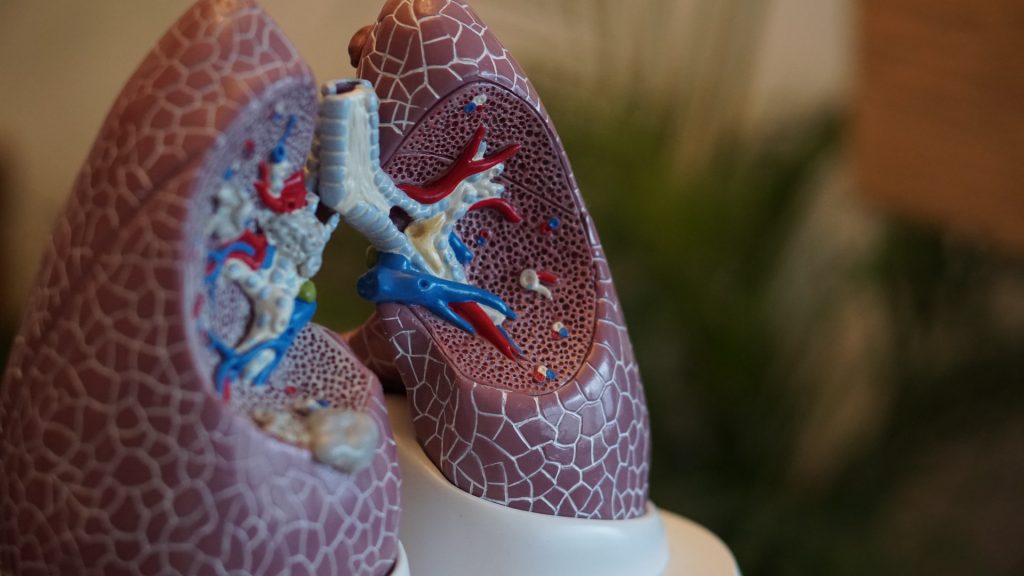
The microorganisms deep in your lungs may play an important role in your overall lung health. And for children undergoing bone marrow transplants, measuring the microbes in their lungs could help predict treatment outcomes, according to a recent study my research team and I published.
What is the lung microbiome?
The microbiome comprises all the microorganisms in the human body, including bacteria, viruses and fungi. The more well-known and commonly studied microbiome is that of the gut.
But recent studies show that the lungs also have a complex and dynamic collection of microbes in combination with the mouth, nose and stomach. Healthy lungs have a baseline level of microorganisms that train them how to mount an immune response against their harmful counterparts. Imbalances in the lung microbiome, or dysbiosis, are associated with poor lung health in children and adults, as well as a variety of diseases that include cystic fibrosis, asthma and chronic obstructive pulmonary disease.
Lung microbes and bone marrow transplants
Optimal lung health is especially important for children about to undergo a bone marrow transplant to treat incurable blood diseases such as leukemia. Also called a hematopoietic cell transplant (HCT), this procedure offers a “hard reset” that uses chemotherapy to wipe out all the patient’s blood cells before replacing them with a new set of donor blood cells.
The problem is that HCT puts a lot of stress on the entire body, and about 12% to 39% of patients develop life-threatening infections and organ dysfunction, often affecting the lungs. Pulmonary disease accounts for 16% of deaths after this procedure in kids. Therefore, making sure the lungs are as healthy as possible before the procedure is important to ensuring success.
My research team and I were interested in discovering how the pulmonary microbiome might relate to lung health in children preparing to undergo this kind of transplant. To do this, we had 104 children breathe into a machine to test their lung function. Then, we measured the composition of their lung microbiome through a bronchoalveolar lavage. This process circulates a saline solution through the lungs of a patient under sedation. We then examine the fluid under a microscope and sequence the genomes of any microbes it contains to identify what types of microorganisms are present.
We found that patients with lungs depleted of their normal bacteria had higher amounts of potentially harmful bacteria that aren’t usually present in healthy lungs. Patients with depleted lung microbiomes also had worse lung function, including signs of scarring, trouble absorbing oxygen and damage at the cellular level.
This study also confirms our previous finding that children with depleted lung microbiomes are two to three times more likely to die from bone marrow transplantation than children without depleted microbiomes. Knowing the composition of the lung microbiome allowed us to more accurately predict who would survive the treatment procedure better than lung function tests alone.
We don’t yet know whether microbiome depletion causes or results from lung disease. But our study suggests that the lung microbiome may be important in predicting bone marrow transplant outcomes. Ultimately, we hope to use this information to develop treatments that restore or strengthen the lungs of high-risk children before they undergo transplantation.
[Get fascinating science, health and technology news. Sign up for The Conversation’s weekly science newsletter.]![]()
Matt Zinter, Assistant Professor of Pediatrics, University of California, San Francisco
This article is republished from The Conversation under a Creative Commons license. Read the original article.





















